28 August 2023
I’ve been gassy before but not like last night. Not with diarrhea at the same time. The only thing I can think that caused it was the new prescription of Budesonide. I was busy on the toilet until 11 pm. Then it was toss and turn scared it would return any moment. I finally drifted off around midnight. Then I waked at 4:30 am and ready to go. I figure I need to leave for my appointment with Dr. Velez around 8:15-8:20. There’s no telling what traffic will be like and on a good day it takes around 20-30 minutes. I-95 always keeps you guessing.
I’ve made a ham sandwich, sliced some apples, and have a supply of Tootsie Rolls to hold me for every how long they keep me. The schedule has me for 3 hours but the first infusion ran to 6 hours. Part of the reason was the nausea I had with the Taxol. I took my anti-nausea medicine last night (I barely remembered it) so I should be good for the first part of the infusion with Herceptin.
9:30 am. I didn’t need to be at Holy Cross for the 9:05 am appointment with Dr. Velez. He schedules it in case but he’ll always come see me during the infusion. They took me back exactly at 9:30 am for the infusion. I keep getting more and more information. Today is only Taxol and not Herceptin. I’m on a 3 week schedule with Herceptin for a total of one year. Taxol will be every week for nine weeks.
Around 10 am Dr. Velez stopped by. We discussed my diarrhea and agreed to keep on the Imodium double dose until the diarrhea abates and then cut back to the normal dose. He also said to keep taking the Budesonide for at least a week. He listened to my bowels with his stethoscope and even palpated my abdomen. It’s a good thing he didn’t listen to them last night. It was like a thunderstorm going off inside of me. He continued to reinforce to keep him posted on my condition via text and to keep an eye on my blood sugar (189).
Jullianne is my nurse again. She’s got a great attitude and is seemingly always up. The first thing is to insert the IV into my port and then clear the port. Next comes a blood draw. She always says it takes an hour for the blood test to come back but it was already in my mail box 30 minutes later. She also let me know the Taxol would take about 1 1/2 hours and I’m waiting for her to start it up.
They ran three blood tests this morning: Comprehensive Metabolic Panel, CBC with Differential and for some reason Dr. Arnaout did a magnesium test. That’s peculiar – not the test – but that he’s no longer my doctor.
The Comprehensive Metabolic Panel tests 19 different parameters.
| Test | Function | Normal Range | My Results |
| Sodium | Determines too much or too little in blood | 136-145 moles/L | 143 |
| Potassium | Electrolyte in blood | 3.5-5.1 moles/L | 4.4 |
| Chloride | Electrolyte in blood | 96-106 milliequivalents/L | 109 |
| CO2 | Affects respiration | 21-31 mmol/L | 26 |
| Anion Gap | Determines acid/base of blood | 5-15 | 8 |
| Glucose | Sugar in blood | 74-109 mg/dL | 184 |
| BUN (Blood Urea Nitrogen) | Blood Urea Nitrogen in blood | 7-25 mg/dL | 13 |
| Creatinine | Measures kidney function | 0.70-1.30 mg/dL | 1.10 |
| eGFR (estimated Glomerular Filtration Rate) | Estimated glomerular filtration rate has a read on kidney health | >=60mL/min/1.73m2 | 70 |
| BUN/Creatinine Ratio | High means not enough blood flow to kidneys | 6.0-20.0 | 11.8 |
| Calcium | Affects bone, kidneys, parathyroid | 8.6-10.3mg/dL | 9.1 |
| AST (SGOT) – Aspartate Transaminase; Serum Glutamic Oxaloaceate Transaminase | Glutamic-oxaloacetic transaminase (liver function monitor) | 13-39 unit/L | 20 |
| ALT (SGPT) – Alanine Transaminase; Serum Glutamic Pyruvic Transaminase | Alanine aminotransferase (liver function) | 7-52 unit/L | 21 |
| Alkaline Phosphatase | Monitor for liver and bone disease | 34-104 unit/L | 63 |
| Total Protein | Measures albumin and globulin. High levels indicate infection | 6.4-8.9 g/dL | 6.8 |
| Globulin, Total | High levels indicate infection | 1.4-3.9 g/dL | 2.6 |
| A/G Ratio (Albumin/Globulin) | Albumin compared to globulin. | >1.0 | 1.6 |
| Total Bilirubin | Liver function | 0.3-1.0 mg/dL | 0.5 |
| Albumin | High levels indicate infection | 3.5-5.7 g/dL | 4.2 |
CBC (Complete Blood Count) with Auto Differential
| Test | Function | Normal Range | My Results |
| WBC | White blood cells – measures leucocytes, a function of immunity | 4.5-11.0K/mcL | 5.3 |
| RBC | Red blood cells – determine amount of oxygen in blood | 4.30-6.20 M/mcL | 3.77 |
| Hemoglobin | Indicator of amount of oxygen in blood | 14.0-18.0 g/dL | 11.3 |
| Hematocrit | How much of your blood is red blood cells | 39.0-55.0% | 33.8 |
| MCV (Mean Corpuscular Volume | Average size of your red blood cells | 80-100.0 FL | 89.5 |
| MCH (Mean Corpuscular Hemoglobin | Amount of hemoglobin, thus oxygen carrying capacity | 27.0-34.0 pct | 29.9 |
| MCHC (Mean Corpuscular Hemoglobin Concentration | Measures bloods ability to carry oxygen | 31.0-37.0g/dL | 33.4 |
| RDW (Red Blood Cell Distribution) | Red cell distribution compares volume with size or red blood cells | 12.0-15.0% | 12.5 |
| Platelets | Count of platelets which affects ability for blood to clot | 130-400 K/mcL | 229 |
| Lymphocytes relative | Measures relative amounts of B and T cells (immunity) | 15.0-40.0% | 8.9 |
| Neutrophils, relative | Tells you your body is under stress | 40.0-65.0% | 88.6 |
| MPV (Mean Platelet Volume) | Measures average size of platelets | 6.2-12.1 FL | 8.8 |
| Monocytes, relative | Measures amount of this white blood cell (immunity) | 1.0-10.0% | 2.2 |
| Eosinophls relative | Measures of amount of white blood cells (immunity) | 0.0-4.0% | 0.1 |
| Basophils, relative | Measures amount for infection/parasites | 0.0-2.0% | 0.2 |
| Neutrophils absolute | Specific amount of this white blood cell in your body | 1.80-7.70K/mcL | 4.70 |
| Lymphocytes absolute | Specific amount of this white blood cell in your body | 1.o0-4.00 K/mcL | 0.50 |
| Monocytes absolute | Specific amount of this white blood cell in your body | 0.20-1.00 K/mcL | 0.10 |
| Eosinophils absolute | Specific amount of this white blood cell in your body | 0.00-0.69 K/mcL | 0.00 |
| Basophils absolute | Specific amount of this white blood cell in your body | 0.00-0.19K/mcL | 0.00 |
| NRBC (Nucleated Red Blood Cell) | Rbc’s are typically enucleate – high values are signs of infections/diseases, cancer | 0.0-0.9% | 0.1 |
Magnesium
The magnesium normal is 1.0=2.7 mg/dL. Mine is 1.5, so it was low. It indicates weakness, irritability, abnormal heart rhythm, nausea and/or diarrhoea, or if you have abnormal calcium or potassium levels.
Regardless of the out of wack levels, everything seems to be OK to proceed with the therapy. First up was magnesium. It’ll take about an hour and then 1 1/2 hours for the Taxol. If no nausea, I should be out of here by 2 or 3 pm. I seem to be doing a consistent 5-6 hours at this place. Good thing the people are nice.
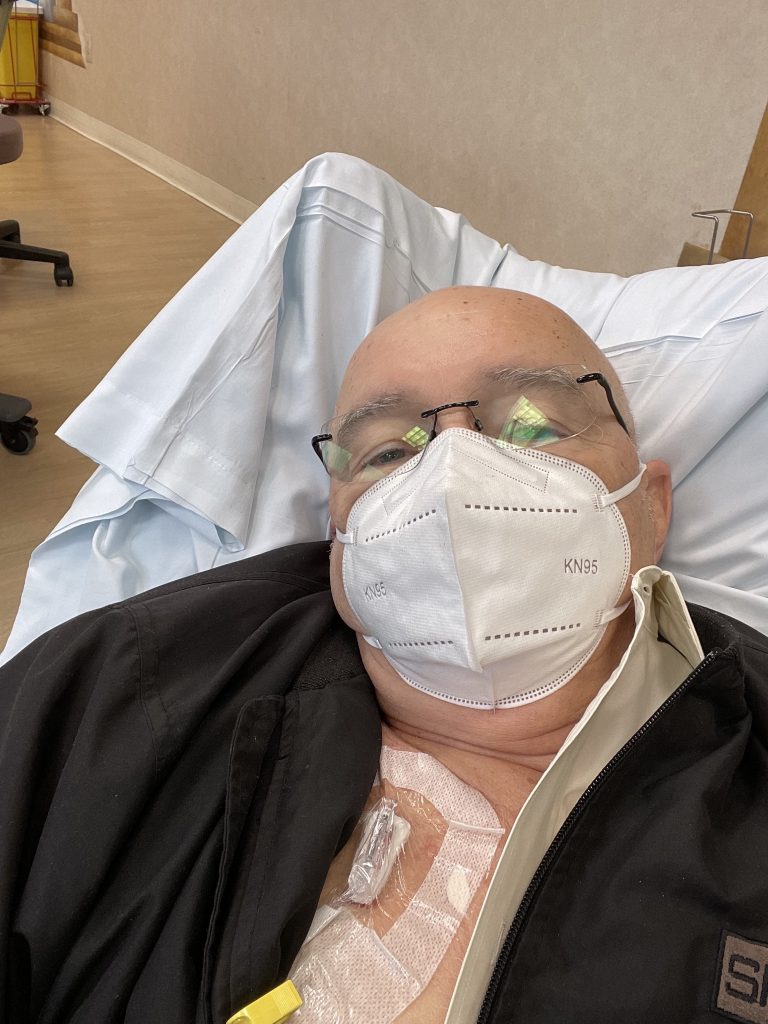
The pro-drug cocktail administered first was the usual suspects. Something for nausea )Dexamethazone) something to line my stomach (Pepside) Benadryl to offset the effects of Taxol and Zofram (another anti-nausea drug). Benadryl makes me sleepy so I cranked the chair back and immediately popped out the needle in my port. The IV lines got caught in the arm of the chair.
A nurse came and immediately asked if I got any of the solution on me. I couldn’t detect any. I imagine it would be classified as a chemical spill for them. It would be just like me to have to call a hazmat team and shut the facility down.
They replaced the IV with a new needle and line and I’m back on schedule. Jullianne started the Taxol very slowly – I suspect because of the nausea the previous time and that prevented any real spill. I was watching the Taxol IV and it was dripping once every 18 seconds. You can program the drip to speed up after a period of time and now I’m racing along at a drop every 6 seconds.
The PA system is hooked into the main hospital across the street. Today we’ve had a potential stroke in one of the rooms of the hospital and we’ve had an emergency in the infusion center (other side of me) for some reason. It’s interesting what is broadcast for everyone to hear.
The IV sounded the alarm that Taxol had finished at 1:59 pm. Now to get unhooked and drive home. I’m also waiting for a call from Walgreens to pick up the remainder of the prescription. There was no nausea with the Taxol this time!
Dr. Velez has already scheduled me for a hydration infusion on Wednesday at 3:30 pm. I hope I don’t have chem fog again and miss it.
Stay tuned!
